A few days ago, a friend casually asked what I do for a living. I told him about a workshop I had just conducted with children who have special needs—children who laugh freely, think deeply and navigate the world in beautifully unique ways.
He glanced at me and said, “Oh, I’ve seen kids like that. Honestly, they’re retards. Everyone thinks it, nobody says it.”
There it was. A single sentence, casually delivered, steeped in ignorance—and heavy with the weight of every stigma that still shadows neurodivergence in our society.
I paused. Then I explained that my work is about supporting children who learn, communicate, and experience the world differently, not less. His words, no matter how “casual,” reduce complex, capable individuals to a slur. That which he called honesty was, in truth, a refusal to understand. And this is where the real problem begins: our language becomes our lens. Words that are thrown around thoughtlessly become walls that block empathy, delay early support, and isolate families when they need community the most.
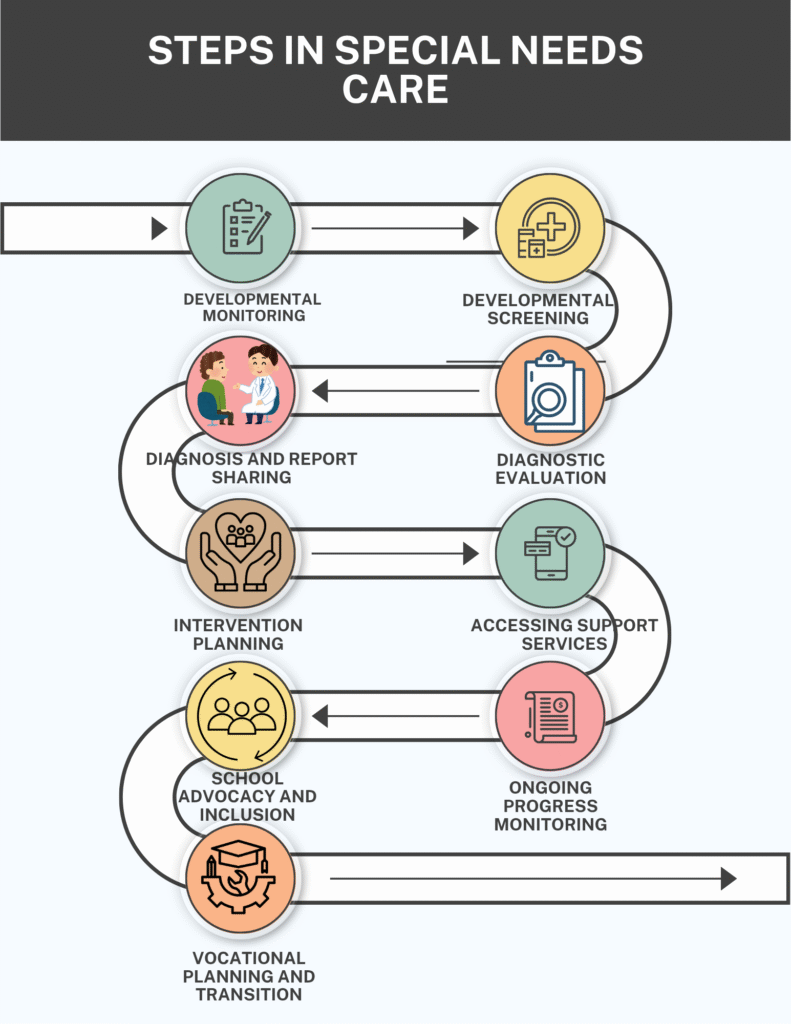
In India, where conversations about disability are often shrouded in shame, this casual cruelty has real consequences. Concerns about development are brushed aside, screenings are delayed, and red flags are ignored—not because the signs aren’t there, but because society isn’t. From the time missed milestones and unusual behaviors are ignored, families begin a long, often confusing path through developmental monitoring, formal screenings, clinical diagnosis, and intervention planning.
In India, this path is not a linear one. Public healthcare lacks the outreach and consistency needed. Private services offer speed but at a cost inaccessible to most. Then comes the search for therapists, inclusive schools, special educators, shadow support, and eventually, vocational training or life skills transition—a system without a single map or guide.
What they deserve instead is clarity, dignity, and compassion. And that can only be done when society chooses to look beyond labels and build bridges instead: from awareness to access, from screening to support, from stigma to strength. It starts with how we speak. It begins with what we choose to see.
1. Developmental Monitoring or the “Wait and Watch Trap“
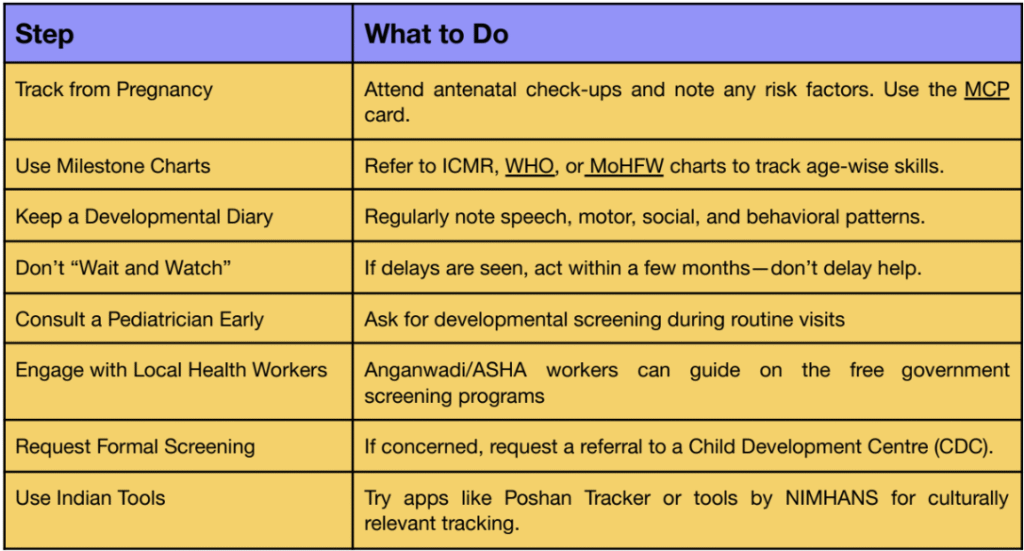
Developmental monitoring in India often begins quietly, sometimes unknowingly, long before a child is born. It starts when an expecting mother visits an Anganwadi center, a government PHC, or a private clinic for her check-ups, where fetal movements, maternal nutrition, and basic health parameters are observed. It continues after birth, in the way a mother instinctively watches her baby’s first smile, or how grandparents recall what age their other children sat up or spoke their first words. In many Indian households, this monitoring isn’t always a formal process—it’s a natural part of caregiving, shaped by family experience, culture, and sometimes worry.
While it’s true that each child develops at their own pace, there is a general timeline of developmental milestones that guides what to expect and when. Even though developmental milestones tracking isn’t a standard practice in India, it’s high time to take it seriously.
2. Practical Steps for Early Developmental Tracking (Indian Context)
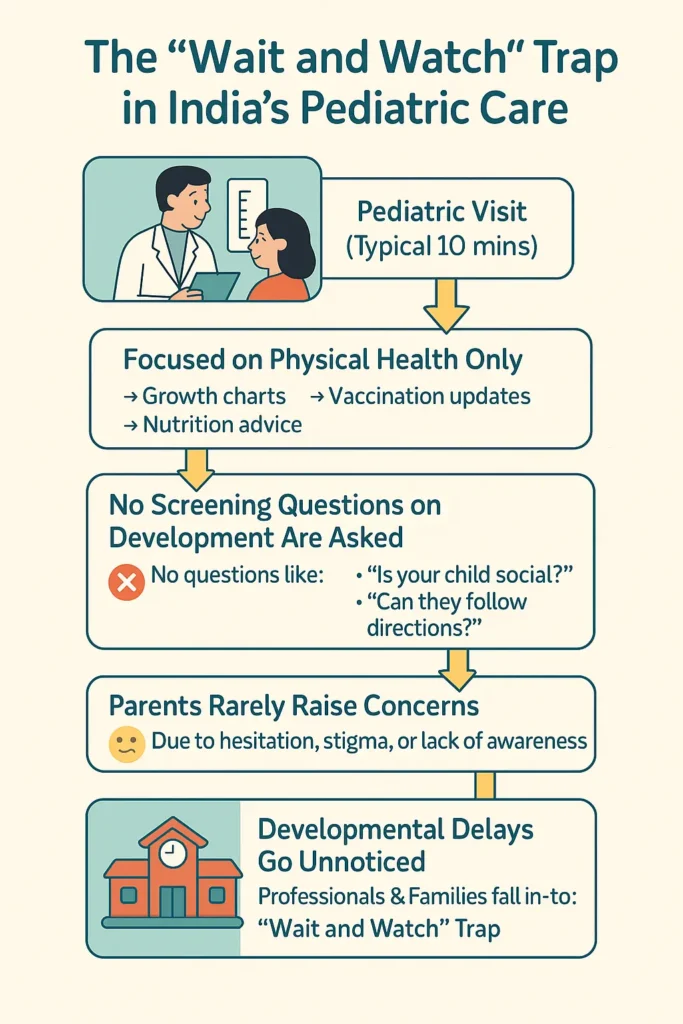
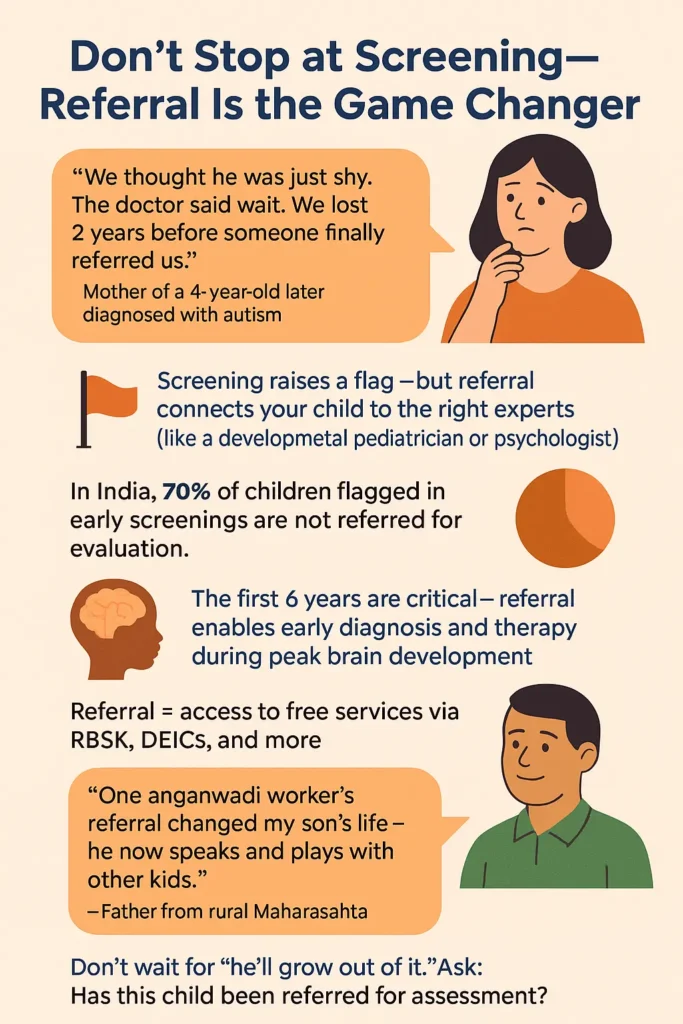
Development screening, on paper, is the very first step in identifying whether a child may need further evaluation for a developmental or learning condition. Developmental screening is the bridge between noticing a concern and truly understanding what that concern might mean. Unlike monitoring, which is ongoing and informal, screening is a structured process—one that utilizes validated tools to assess whether a child’s development is on track.
When a screening raises concerns, it helps parents recognize that something might need closer attention. It also sets the stage for timely recommendations, referrals, and early interventions that can make a meaningful difference in a child’s journey.
2.1. Overview of Screening Types for Children (India Context)
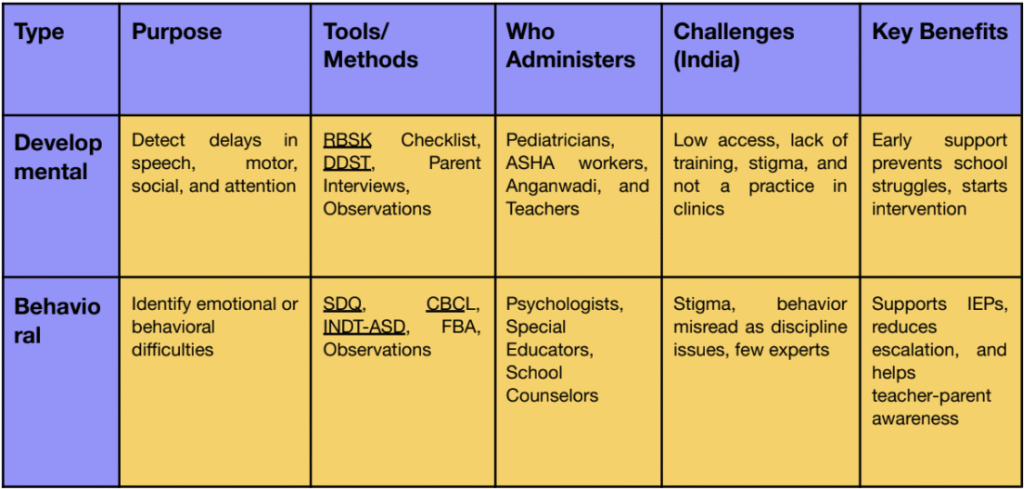
Screening, whether conducted by a psychologist or a pediatrician, sets the parent on the right track to seek the appropriate referral or clarification on what to expect, outcomes, and a suitable referral.
3. Diagnostic Evaluation
Once a concern is raised about a child’s development or learning after screening, a diagnostic evaluation is next—a process that may feel daunting but is vital. In India, nearly 1 in 10 children is estimated to have a developmental or learning challenge, yet most remain undiagnosed or misdiagnosed due to stigma, lack of access, or delayed action.
Diagnostic evaluation is the systematic process of identifying and understanding the nature and extent of a child’s developmental, cognitive, emotional, or physical challenges. A diagnostic evaluation is more than just a label—it’s a structured, 3-step process:
3.1. Analysis
Information is gathered from multiple sources—parent interviews, teacher reports, medical history, and direct observations. This helps build a complete picture of the child’s functioning.
3.2. Evaluation
The child is assessed using standardized tools and informal methods by professionals like psychologists, speech therapists, and occupational therapists to check skills across domains (language, motor, behavior, cognition, etc.).
3.3. Diagnosis
Based on the results, a formal diagnosis (e.g., autism, ADHD, developmental delay) is made. This diagnosis helps decide the type of support or intervention the child needs.
It is a crucial step in determining whether a child has special needs and what type of support or intervention they require.
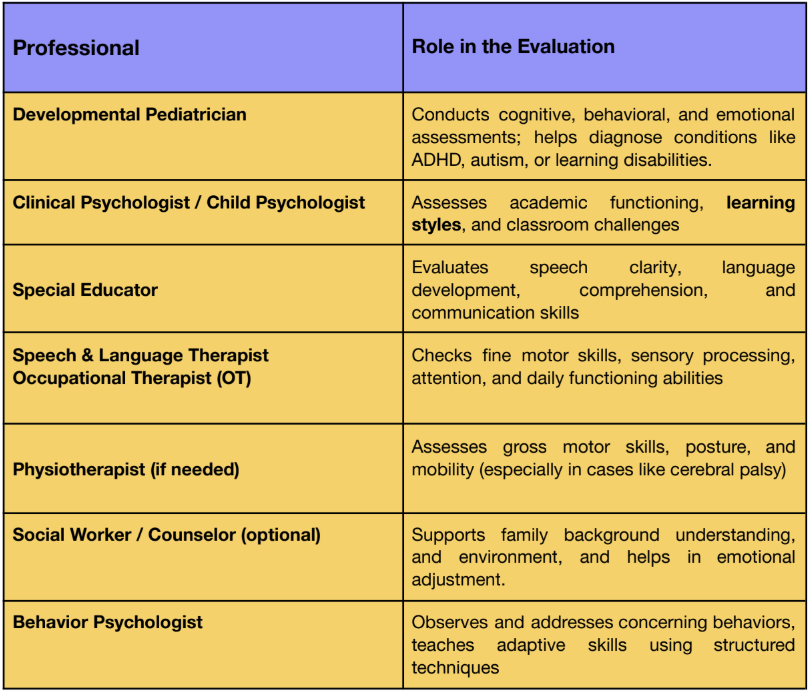
In India, diagnostic evaluations are typically conducted by multidisciplinary teams comprising pediatricians, psychologists, special educators, speech therapists, and occupational therapists.
3.4. Professionals Involved in Diagnostic Evaluation (India)
4. Diagnosis and Report Sharing
Following the administration of standardized assessments and the collection of multi-source inputs—including developmental history, medical evaluations, parent interviews, teacher observations, and classroom performance—the clinical psychologist synthesizes the findings to arrive at a formal diagnosis. In India, this process typically adheres to diagnostic criteria outlined in the DSM-5 or ICD-10, depending on institutional practice.
The clinical psychologist plays a pivotal role not only in delivering the diagnosis but also in offering psychoeducation to families. This involves:
● Explaining the nature of the identified condition (e.g., Autism Spectrum Disorder, ADHD, Specific Learning Disability)
● Addressing parental concerns and misconceptions
● Guiding the family on available therapeutic, educational, and medical interventions
● Referring them to relevant specialists such as occupational therapists, speech-language pathologists, special educators, and developmental pediatricians
The psychologist also ensures that a detailed diagnostic report is provided. This typically includes:
● Background history
● Assessment tools used and interpretation of results
● Observations across home and school settings
● Diagnostic conclusion
● Recommendations for intervention and educational planning
This report becomes the foundation for developing Individualized Education Plans (IEPs) by special educators in schools and CDCs, availing disability certification (if applicable) under the Rights of Persons with Disabilities Act, 2016, and securing school-based accommodations under CBSE or other educational boards.
In the Indian context, the diagnostic report not only serves as a clinical tool but also acts as a navigation guide for the child’s educational and developmental journey, especially in systems where early intervention is still emerging as a structured service.
4.1 Common Diagnoses in India: A Cultural Lens
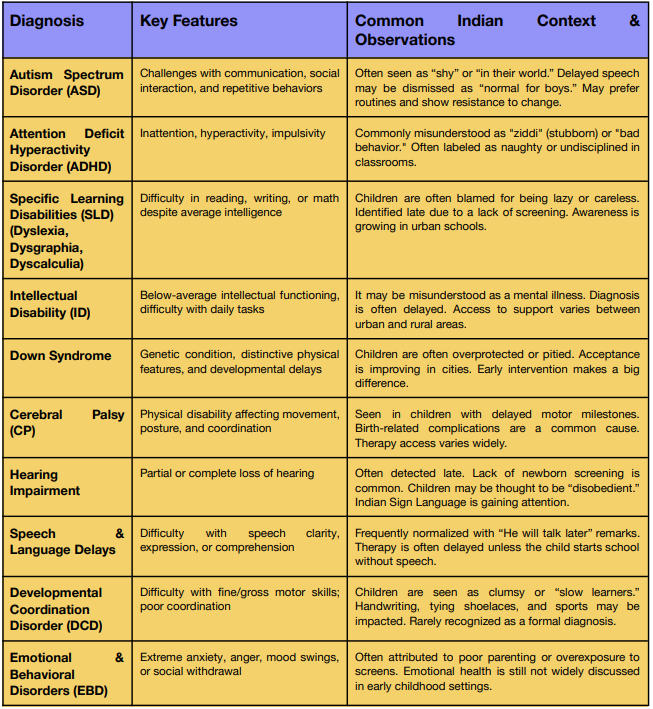
The developmental journey of a special needs child starts with diagnosis. For many parents, getting a diagnosis may feel like the ground has shifted, but what it truly offers is direction. It puts a name to the unknown. That moment, even though overwhelming, is not a conclusion but a compass.
The next chapter, intervention, is just as important and we are here to guide you through it all. It involves building a circle of care around the child, about understanding the therapies, educational strategies, and daily adjustments that can help them thrive.
Let us support you through every step. Contact us: reachout@kidable.in or +91 9266688705
Merlin Joseph
founder
Wellness Coordinator at KidAble who believes mental health should be a child’s foundation, not an afterthought. She brings empathy and insight to every session, helping young minds build confidence, expression, and emotional balance.

