Imagine sitting in a classroom during storytime. The teacher begins reading a book aloud, but one child keeps fidgeting in their seat, looking around, and whispering to their classmate. When asked a question about the story, they don’t remember what was read. They later wander to the bookshelf without permission, accidentally knock over a pile of books, and then get scolded for “not listening again.”
Now picture another child in the same classroom. This child has heard “Sit properly,” “Stop fidgeting,” and “Why can’t you focus like the others?” so many times that they’ve learned to sit still and avoid attention. On the surface, they appear calm but inside, they might be feeling anxious, overwhelmed, or even ashamed. They’re trying so hard to ‘fit in,’ but that effort takes a toll. These are children who may be masking their struggles, and their challenges often go unseen.
You might think the child is just misbehaving or not paying attention. But what if they’re genuinely trying and struggling? Maybe they didn’t sleep well or are anxious, hungry, or their mind has wandered off to a completely different, imaginative part of the story, creating a whole world of their own.
In many Indian classrooms or homes, these children hear remarks like “He’s always distracted” or “How will you manage in a big school?” These comments overlook the complex inner experience of the child and set overgeneralised expectations on their behavior. Sometimes, these behaviors are situational but when they persist across settings like home, school, playground and significantly interfere with learning and daily functioning, professionals consider conditions like ADHD.
Their brains may be wired differently, but different doesn’t mean less. With early identification and right support, many children with ADHD grow to be imaginative problem-solvers, enthusiastic leaders, creative thinkers, and compassionate peers.
What is ADHD in Children?
ADHD (Attention-Deficit/Hyperactivity Disorder) is a neurodevelopmental condition that affects how the brain manages attention, energy levels, and impulse control. ADHD presents in three primary types: inattentive, hyperactive-impulsive or combined.
In everyday life, this can look like:
Difficulty staying focused on one thing
Trouble sitting still for long periods
Acting without thinking (impulsivity)
Common ADHD Symptoms in Children

These symptoms usually appear before age 12 and are seen in more than one setting (like both school and home). While ADHD is diagnosed in childhood, it doesn’t simply go away with age, many individuals continue to experience symptoms into adolescence and adulthood.
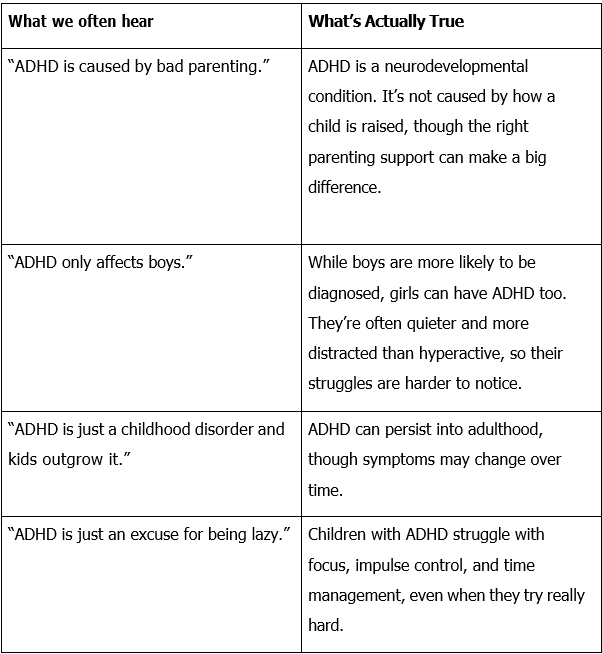
Myth: ADHD is just ‘bad behaviour’
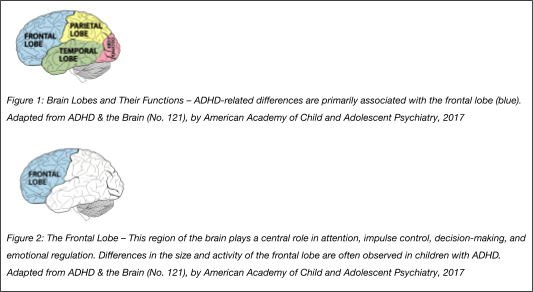
Scientific research using brain imaging has shown that some areas of the brain in children with ADHD may be smaller or mature differently compared to children without ADHD.
These differences are especially noticeable in the frontal lobe, which is the part of the brain responsible for attention, memory, judgment, impulse control, social behavior, decision-making, and emotional regulation. (American Academy of Child and Adolescent Psychiatry, 2017)
These differences can explain why everyday tasks like staying focused, waiting or finishing homework feel much harder.
ADHD Myths vs. Reality
ADHD Treatment in India
The most effective treatment for ADHD is a combination of behavioral therapy, and occupational therapy. While medication can be helpful, they are usually recommended only when a child is experiencing significant distress or daily functioning is seriously impacted. Many children benefit greatly from non-medication approaches, especially in the early years.
Behavioral Strategies That Work:
Clear routines: A predictable daily schedule helps reduce confusion and stress.
Visual checklists: Useful for organising tasks and steps (like brushing teeth or packing a bag).
Positive reinforcement: Praising and rewarding effort and not just outcomes can help build self-esteem. For example: saying “You worked so hard to finish your homework!” or giving access to a favorite toy.”
Structure and limits: Simple rules and consistent consequences can help reduce overwhelm. For example: A visual “house rules” chart with simple pictures or symbols can make expectations easier for children to understand and follow.
Other Therapies That Support ADHD
Parent Training Programs: help caregivers understand ADHD and learn strategies to manage behavior consistently.
Social Skills Training: supports children in understanding emotions, taking turns, and building friendships.
Counseling or Play Therapy: helps children express feelings, manage frustration, and build coping skills.
School-based accommodations: allowing for extra movement breaks, longer test times, or a quiet space for learning.
[Also read: Navigating Healthcare with Children – a quick guide to support services and intervention planning.]
ADHD is not a misbehavior problem; it’s a condition that affects how a child thinks, moves, and responds to the world. With increased awareness, especially in Indian
classrooms and homes, we can move from, “Why can’t he just sit still?” to asking, “How can I help?”
Early intervention makes all the difference.
We’re here to support you through every step.
Email us reachout@kidable.in or Call us +91-9266688705

