Diagnosis sets you on a journey of finding the right professionals, asking the right questions, and building your child’s care network. That stage is like crossing a river — challenging, but with a sense of direction.
What comes next is often harder to talk about.
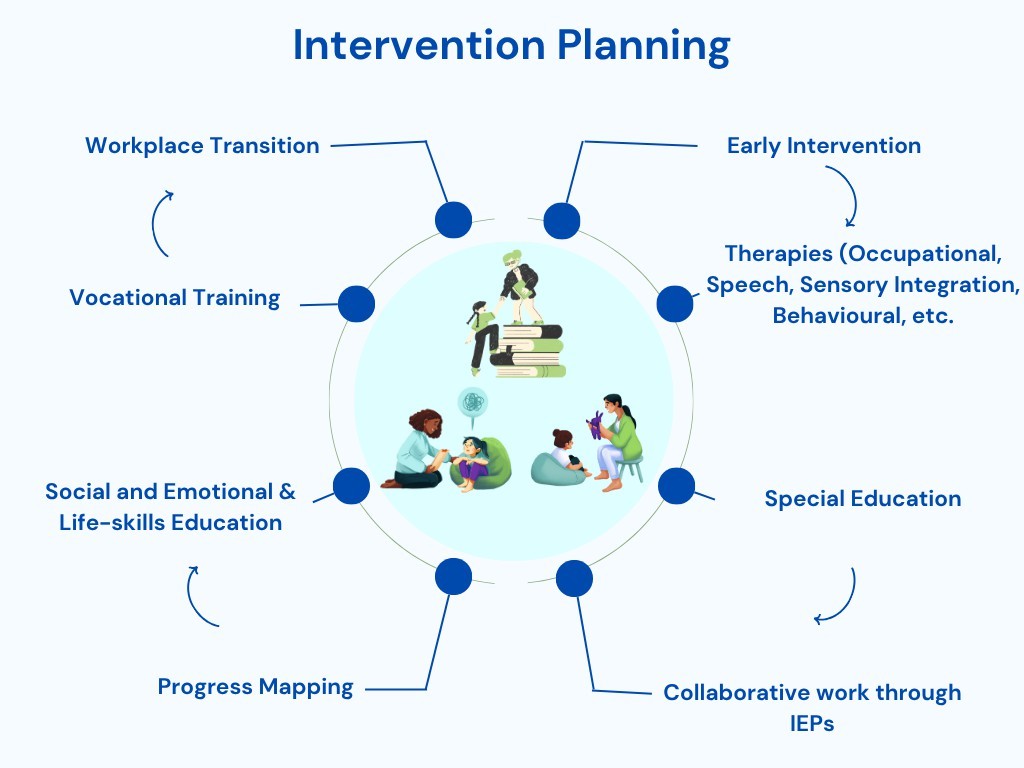
Intervention planning feels more like navigating a flood. There are multiple therapies, shifting routines, and slow or uncertain progress. Some days you move forward. On other days, you feel stuck or unsure. You question, “Does my child even need therapy?” Should I pause therapy? Try something new? Push through?
In India, where access to consistent, coordinated care isn’t always easy, these questions weigh heavier.
Intervention planning feels more like navigating a flood. There are multiple therapies, shifting routines, and slow or uncertain progress. Some days you move forward. On other days, you feel stuck or unsure. You question, “Does my child even need therapy?” Should I pause therapy? Try something new? Push through?
In India, where access to consistent, coordinated care isn’t always easy, these ques
This blog addresses that stage — the emotionally and logistically complex phase that follows diagnosis. It’s about helping you stay steady when things feel scattered. Because even in rising waters, your presence, questions, and effort help shape a path forward for your child and yourself.
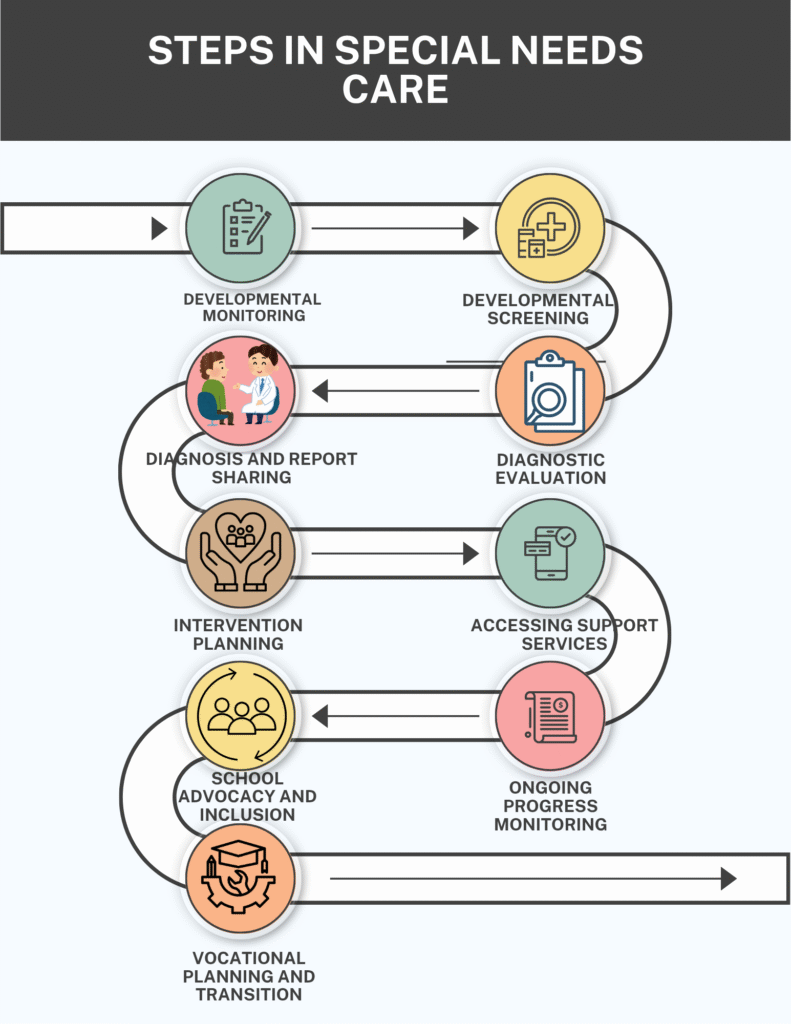
1. Intervention Planning
Let’s say you’ve consulted a reputed psychologist, received a detailed diagnostic report, and the next steps recommend Occupational Therapy, Speech Therapy, and Special Education.
But what now? Most parents find themselves asking:
- What if this is just a phase?
- How many sessions does my child need?
- What does each therapy aim to achieve?
- How will I know if it’s working?
- “I feel like I’m repeating my child’s story over and over — can’t they all just talk to each other”?
- Will therapy cure my child?
This is where intervention planning becomes more than just a next step— it becomes the roadmap to your child’s development.
1.1 Why Intervention Planning Matters
Intervention planning is not a one-time event; it is a dynamic, ongoing process that tailors support to your child’s developmental profile. It:
- Integrates the recommendations from various specialists,
- Ensures consistency across home, school, and therapy settings.
- Helps track progress across developmental domains (motor, cognitive, language, emotional),
- Builds a collaborative ecosystem around the child, with parents as key stakeholders.
In the Indian context, the importance of structured intervention has gained significant momentum, particularly in the last two decades. Recognizing that developmentally diverse children require more than a one-size-fits-all approach. India has taken notable strides in formulating inclusive policies and institutional frameworks that cater specifically to the needs of Children with Special Needs (CWSN).
- The implementation of laws like the RPWD Act of 2016,
- National programs like RBSK, and
- A growing network of therapy centers, special educators, and inclusive schools.
However, collaborative work is truly what makes the difference. In the rush of managing multiple therapies— Occupational Therapy, Speech Therapy, Special Education — it’s easy for parents to treat each session as a separate task. For instance, you might head straight to OT after a good counseling session without sharing recent emotional progress with the next therapist. But when professionals work in silos, the benefits of therapy don’t generalize across settings. Sharing even small achievements— like your child asking a question during a counseling session or using new words at home — can make a significant difference.
Parents are the thread that weaves all these therapies together — sharing insights ensures your child’s progress is not just limited to one room but carried across their whole developmental journey.
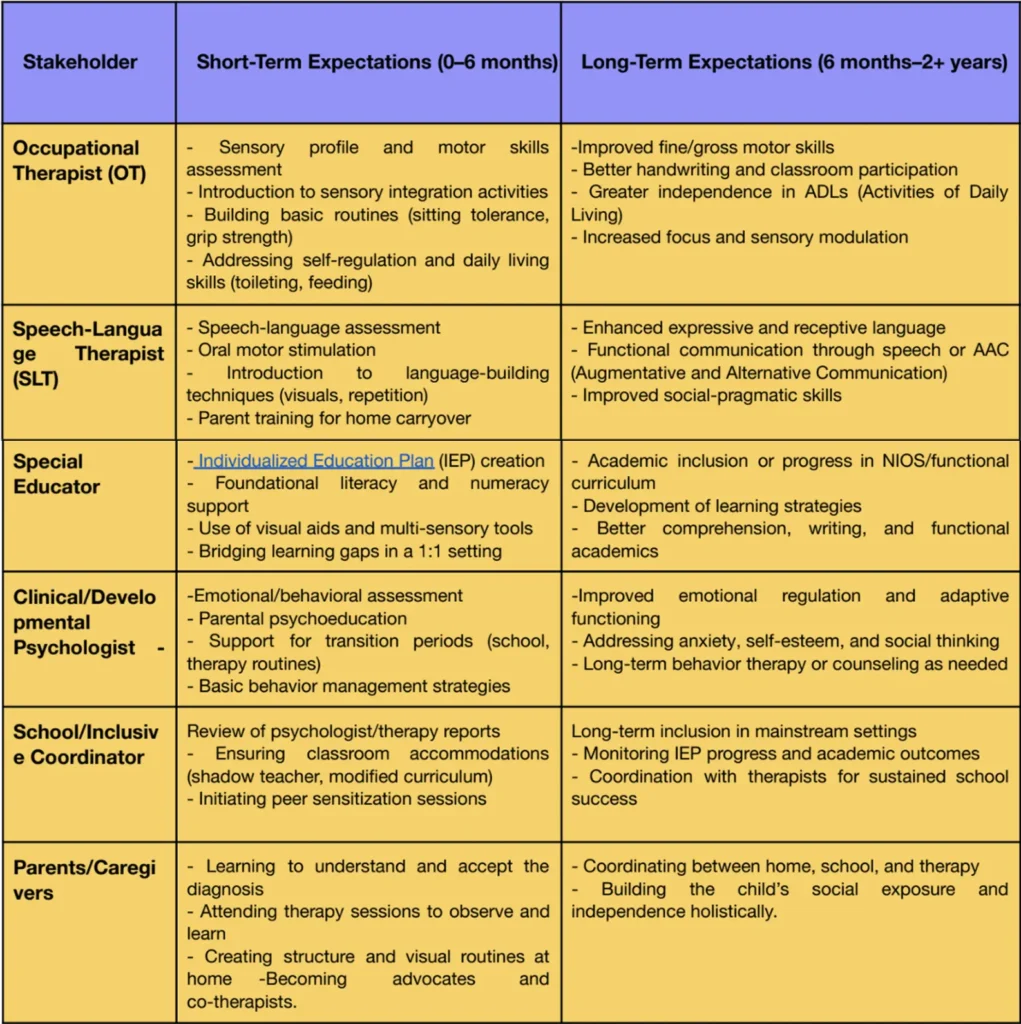
1.2 Therapeutic Outcomes
2. Access to Support Services
The Central Government Health Scheme (CGHS) has outlined recommended therapy session frequencies for children based on their specific diagnoses – namely, Autism, ADHD, and Learning Disability. The Central Government Health Scheme (CGHS) also specifies the required qualifications and certifications for professionals working with Children with Special Needs (CWSN), ensuring that only appropriately trained and accredited therapists provide intervention services.
Once you’ve received a diagnosis and a structured intervention plan from your psychologist — often recommending Occupational Therapy, Speech Therapy, Special Education, or ABA— the next big step is accessing these services effectively.
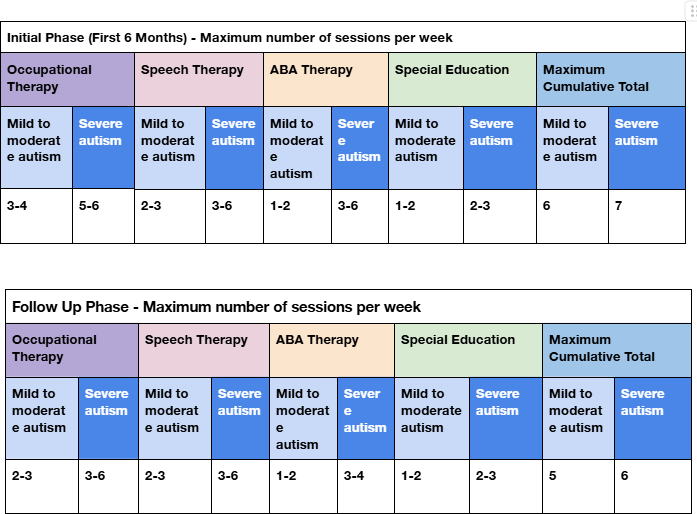
The table above provides a detailed overview of the suggested number of sessions and therapy required for autism.
2.1 Decide Between Public, Private, or Hybrid Services
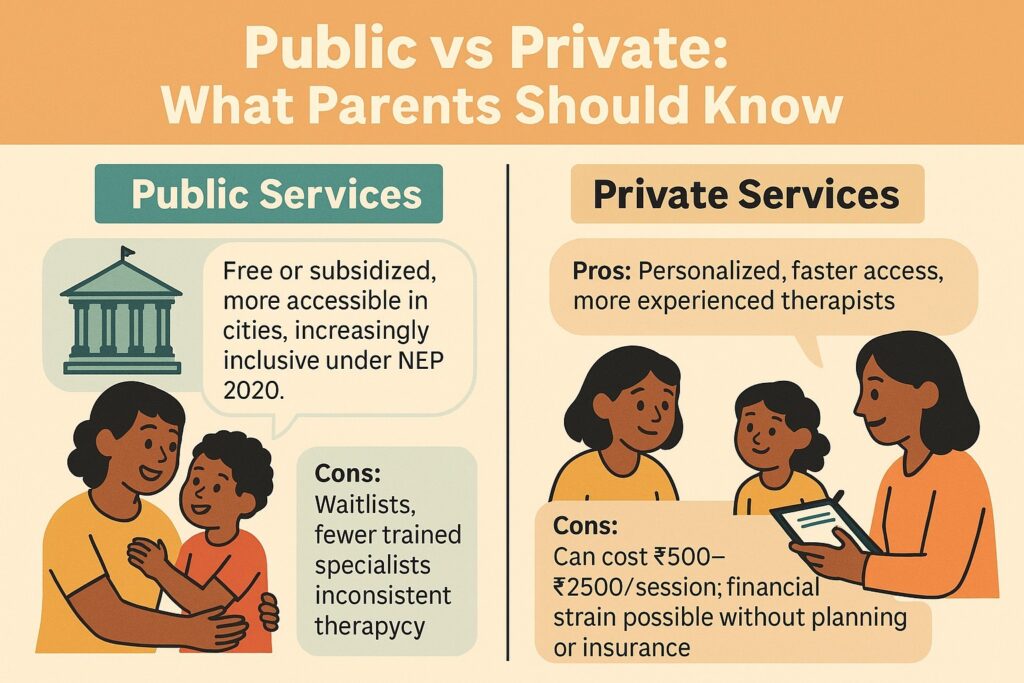
The very first decision to make after receiving an intervention plan is whether to access services through public systems, private providers, or a combination of both.
This choice depends on several factors:
- Availability in your area
- Cost
- Waiting time
- The intensity of support your child requires.
The very first decision to make after receiving an intervention plan is whether to access services through public systems, private providers, or a combination of both.
This choice depends on several factors:
- Availability in your area
- Cost
- Waiting time
- The intensity of support your child requires.
Public services, such as those offered under the Rashtriya Bal Swasthya Karyakram (RBSK), DDRCs, or government hospitals, are often free or subsidized, but they may have long waiting lists and limited individual attention. On the other hand, private services tend to offer faster access and personalized care, though they can be expensive. Many families opt for a hybrid model, using public services for foundational therapies like OT or speech, while turning to private providers for more intensive or specialized support like ABA or special education. This approach balances affordability with effectiveness.
- Public/Government Services (e.g., RBSK, AIIMS, NIMHANS, district hospitals, SSA, DDRCs): Free or subsidized. Limited appointments and long waiting times.
- Private Services (e.g., child development centers, certified clinics, freelance therapists): Immediate access and more personalized care, but can be expensive.
- Hybrid Model: Use public services for foundational support and private therapy for consistency or specialization.
2.2 Make First Contact & Inquire
During your initial conversation, be sure to ask about the session costs and whether there are package options available. Equally important is checking the therapist’s qualifications and their experience with children, ensuring they are certified by relevant bodies such as the Rehabilitation Council of India (RCI), especially for occupational therapy, speech-language therapy, and special education.
2.3 Understand the Therapeutic Approach
Take time to understand the therapist’s approach — whether it’s play-based, sensory-integrated, evidence-based, or eclectic. Also, inquire about the possibility of home programs and whether the therapist is open to sharing updates and collaborating with other professionals involved in your child’s care.
To prevent overwhelm, it’s best to start with one or two core services— typically occupational therapy and speech therapy. Once your child adjusts, additional supports like special education or behavior therapy can be introduced gradually, based on comfort and schedule feasibility.
2.4 Create a Weekly Therapy Calendar
With therapies underway, the next essential step is to create a weekly therapy calendar. Refer to the intervention plan to determine the number of sessions recommended per week — perhaps three OT sessions, two speech sessions, and two special education sessions. While doing this, be mindful not to overload any single day. Spread the sessions across the week, keeping space for free play, downtime, and travel. A visual calendar placed at home can be updated in a smart-watch or phone, so that the child anticipates what’s coming — many children enjoy seeing their “therapy rainbow schedule” displayed on the wall.
2.5 Maintain a Shared Progress Folder
As therapy progresses, it’s vital to maintain a shared progress folder. Keep copies of all assessments, session notes, and progress updates in one place. This folder becomes a powerful tool for collaboration. By sharing relevant updates across professionals— for example, letting the speech therapist know that the child was more attentive after a sensory activity in OT — you help create continuity across therapies. Ideally, set up monthly check-ins where therapists can align on goals and make necessary adjustments.
3. Ongoing Progress Monitoring
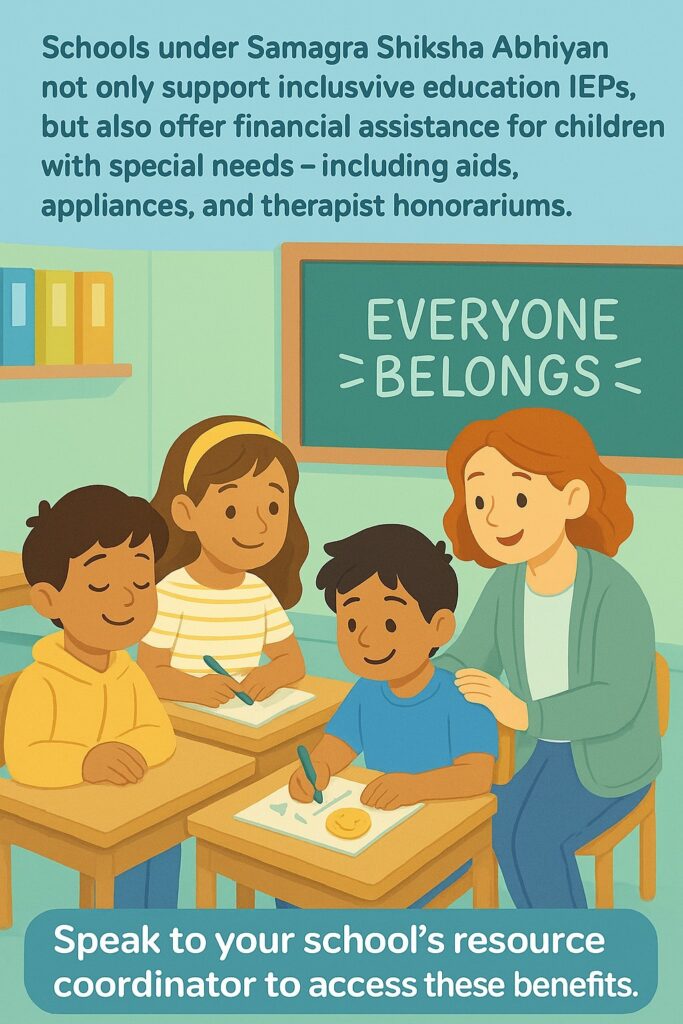
Therapy isn’t a “one-and-done” experience. As your child develops, their needs and strengths change too. That’s why ongoing progress monitoring is so essential. One powerful tool that helps families and professionals stay on the same page is the Individualized Education Plan (IEP). Think of the IEP as your child’s personal growth map— tailored to who they are today, and who they can become. It includes:
- A snapshot of your child’s current skills (not just struggles!)
- Clear goals for learning, communication, or behavior
- Specific services like OT, speech, or special education, and how often they’ll happen
- A way to check in regularly and see how things are going.
4. School Advocacy and Inclusion
Many parents feel anxious when their child with special needs is about to enter or continue in a mainstream school setting.
- Will the teacher understand my child’s needs?
- Will classmates be kind and inclusive?
- Will the school support or ignore our concerns?
These are real, valid questions— and if you’re asking them, you’re already advocating for your child, most importantly, by caring deeply. In the Indian context, most families learn about their child’s condition and developmental differences not from pediatricians, but from school-based professionals — special educators, teachers, or school counselors. These individuals often become the first point of contact for further referrals, assessments, and emotional support. It’s a reminder that school is not just a place of learning, but often a starting point of understanding
4.1 What the Law Says
India’s Rights of Persons with Disabilities (RPWD) Act, 2016 mandates that all children have the right to inclusive education. This means:
- Schools must admit children with disabilities.
- They must provide accommodations: whether that’s modified teaching, assistive devices, shadow teachers, or exam support.
- Children must be treated with dignity and protected from discrimination or exclusion.
But here’s the reality: inclusion doesn’t always happen on its own. It oft
5. Vocational Planning and Transition
As your child enters adolescence, your role begins to shift.
This stage is all about transitioning from therapy to real-world readiness—helping them learn skills that build confidence, independence, and purpose.
This might include:
- Daily living skills: using money, cooking, managing time
- Career exposure: simple tasks, creative arts, computers, hospitality
- Building workplace behavior: following routines, asking for help, and teamwork
- Trial jobs or internships through NGOs or local businesses
There are many wonderful organizations across India offering vocational training, like Muskaan Foundation, Evoluer, Tamana, Sristi, V-Excel, and AFA. Some schools also include transition planning for older students with special needs.
Ask early — around 13 -14 years, is a good time to start.
In India, many parents delay seeking help, even when they sense something is different about their child and most children are first referred for help only after they’ve struggled in school for years.
Deep down, parents know. And often, what holds them back isn’t love — it’s stigma. However, what needs to be learnt is that the earlier we act, the more confident and capable children and parents can feel.
The first six years of life are a golden window for learning. During this phase of rapid brain growth, even simple strategies— like speech therapy, sensory regulation, or emotional coaching — can lead to life-changing progress. A child who gets support early may go on to read, speak, and participate more confidently. Families, in turn, feel less confused and more connected.
Yes, stigma is real. But so is change. Every time a parent speaks up, asks questions, and seeks support, they help create a culture that values understanding over judgment.
You are not alone. And your child is not broken.
How Kidable Can Help
We know what it feels like to sense that something’s different — and not know where to begin. At Kidable, we support families right from the start — whether it’s a toddler not yet using words, or an older child who’s struggling to keep up at school. You don’t have to wait because waiting doesn’t bring answers – early action does. And we take you from waiting and confusion, to answers and actionable steps.
From supporting speech and language development, to helping your child manage sensory sensitivities, or building their ability to express needs through self-advocacy, like learning to say, “This is too loud,” or “I need help,”
Here’s how we support you:
- Developmental Screening (as early as 18 months) to spot challenges before they become roadblocks
- Age- and interest-appropriate goals, so your child builds real-life skills, not just worksheet progress
- Certified professionals, including speech therapists, OTs, and special educators, who understand neurodivergent learning
- Customized intervention planning built around your child’s needs, not a generic protocol
- Parent coaching to help you respond with confidence, not confusion
- Guidance for school inclusion, IEPs, accommodations, and classroom advocacy So your child doesn’t just attend school, but belongs there
Because when support starts early, children don’t fall behind— they grow with the help they need, at their own pace.
Let us support you through every step. Contact us: reachout@kidable.in or +91 9266688705
Merlin Joseph
founder
Wellness Coordinator at KidAble who believes mental health should be a child’s foundation, not an afterthought. She brings empathy and insight to every session, helping young minds build confidence, expression, and emotional balance.

